Page 1 of 6
Summary of Benefits and Coverage: What this Plan Covers & What You Pay for Covered Services Coverage Period: 01/01/2024 – 12/31/2024
Cigna Health and Life Insurance Co.: Cigna Connect Flex Silver 5750 (200-250% FPL) Coverage for: Individual & Family | Plan Type: EPO
The Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would
share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately.
This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, call 1-866-494-2111 or visit us
at www.cigna.com/ifp-documents. For general definitions of common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider,
or other underlined terms, see the Glossary. You can view the Glossary at https://www.healthcare.gov/sbc-glossary/ or call 1-866-494-2111 to request a copy.
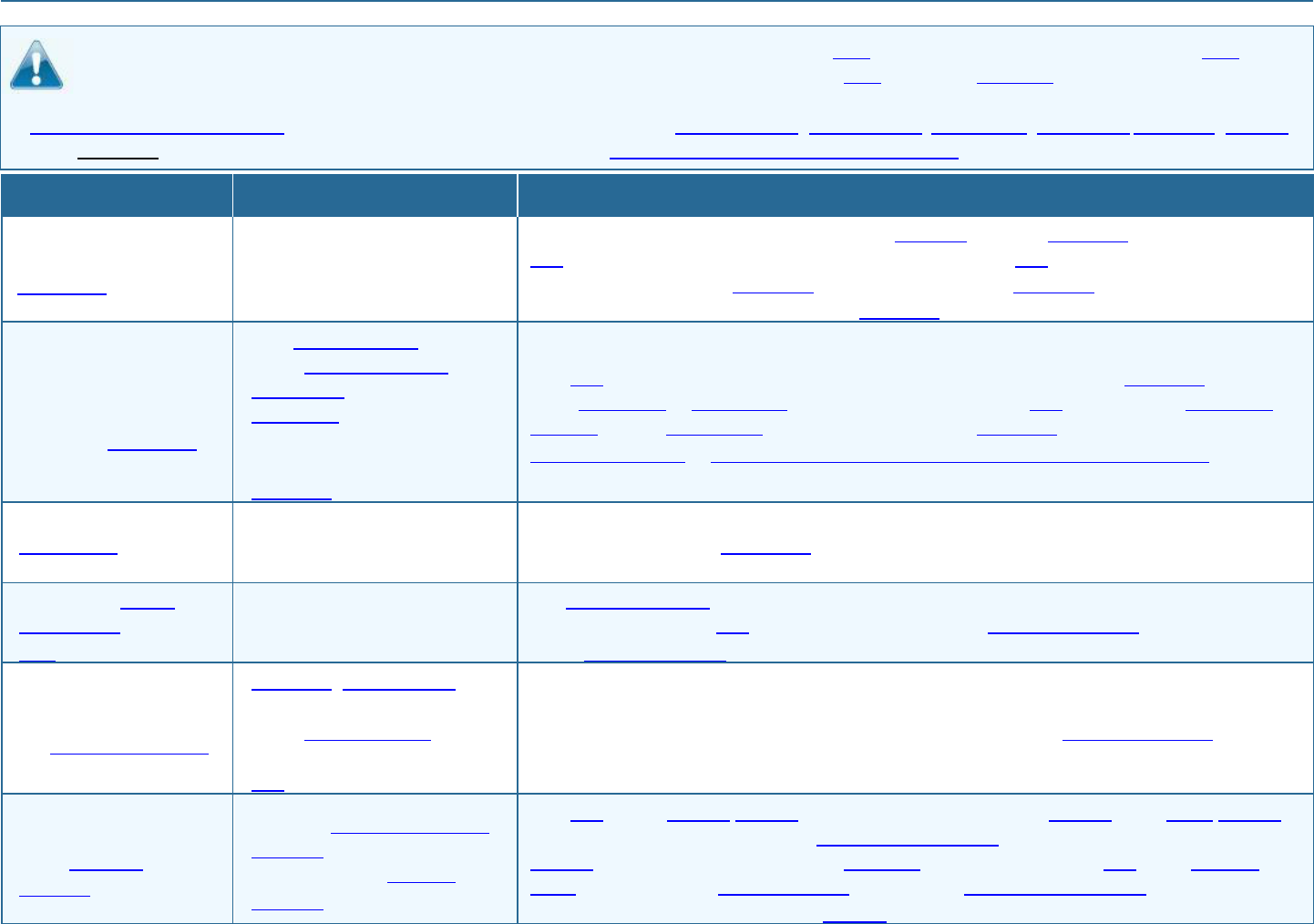
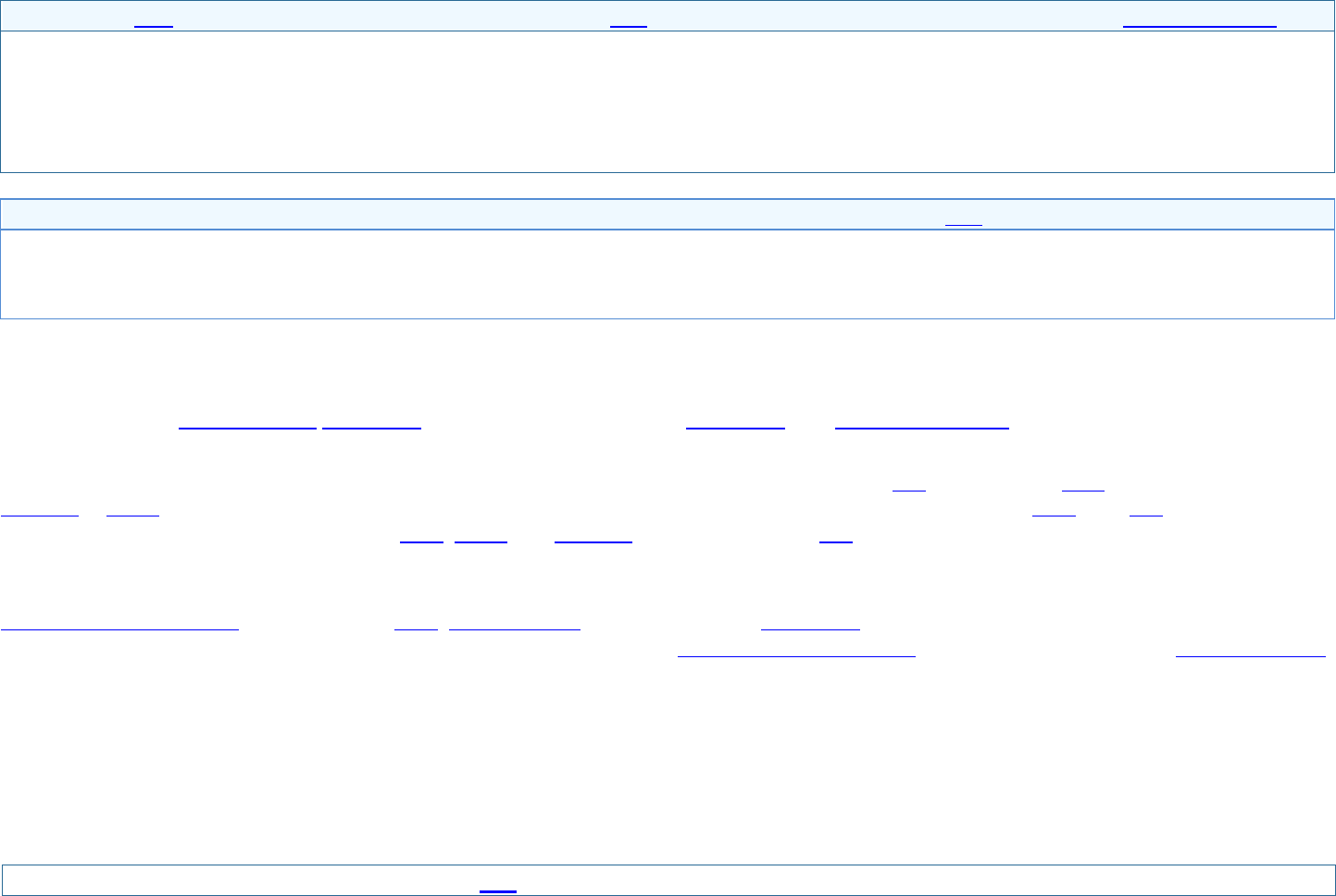
Important Questions
Answers
Why This Matters:
What is the overall
deductible?
$4,000 person/ $8,000 famil
y
Generally, you must pay all of the costs from providers up to the deductible amount before this
plan begins to pay. If you have other family members on the plan, each family member must
meet their own individual deductible until the total amount of deductible expenses paid by all
family members meets the overall family deductible.
Are there services
covered before you
meet your deductible?
Yes. Preventive care, office
visits, Prescription drugs,
Urgent care visits subject to a
copayment and eye
exam/glasses for children are
covered before you meet your
deductible.
This plan covers some items and services even if you haven’t yet met the deductible amount.
But a copayment or coinsurance may apply. For example, this plan covers certain preventive
services without cost-sharing and before you meet your deductible. See a list of covered
preventive services at https://www.healthcare.gov/coverage/preventive-care-benefits/.
Are there other
deductibles for specific
services?
No.
You don’t have to meet deductibles for specific services.
What is the out-of-
pocket limit for this
plan?
$7,550 person/ $15,100 family
The out-of-pocket limit is the most you could pay in a year for covered services. If you have other
family members in this plan, they have to meet their own out-of-pocket limits until the overall
family out-of-pocket limit has been met.
What is not included in
the out-of-pocket limit?
Premiums, balance-billing
charges, penalties for failure to
obtain preauthorization for
services and health care this
plan doesn’t cover.
Even though you pay these expenses, they don’t count toward the out–of–pocket limit.
Will you pay less if you
use a network
provider?
Yes. See www.cigna.com/ifp-
providers or call 1-866-494-
2111 for a list of network
providers.
This plan uses a provider network. You will pay less if you use a provider in the plan’s network.
You will pay the most if you use an out-of-network provider, and you might receive a bill from a
provider for the difference between the provider’s charge and what your plan pays (balance
billing). Be aware, your network provider might use an out-of-network provider for some services
(such as lab work). Check with your provider before you get services.
Page 2 of 6
Important Questions
Answers
Why This Matters:
Do you need a referral
to see a specialist?
No.
You can see the specialist you choose without a referral.
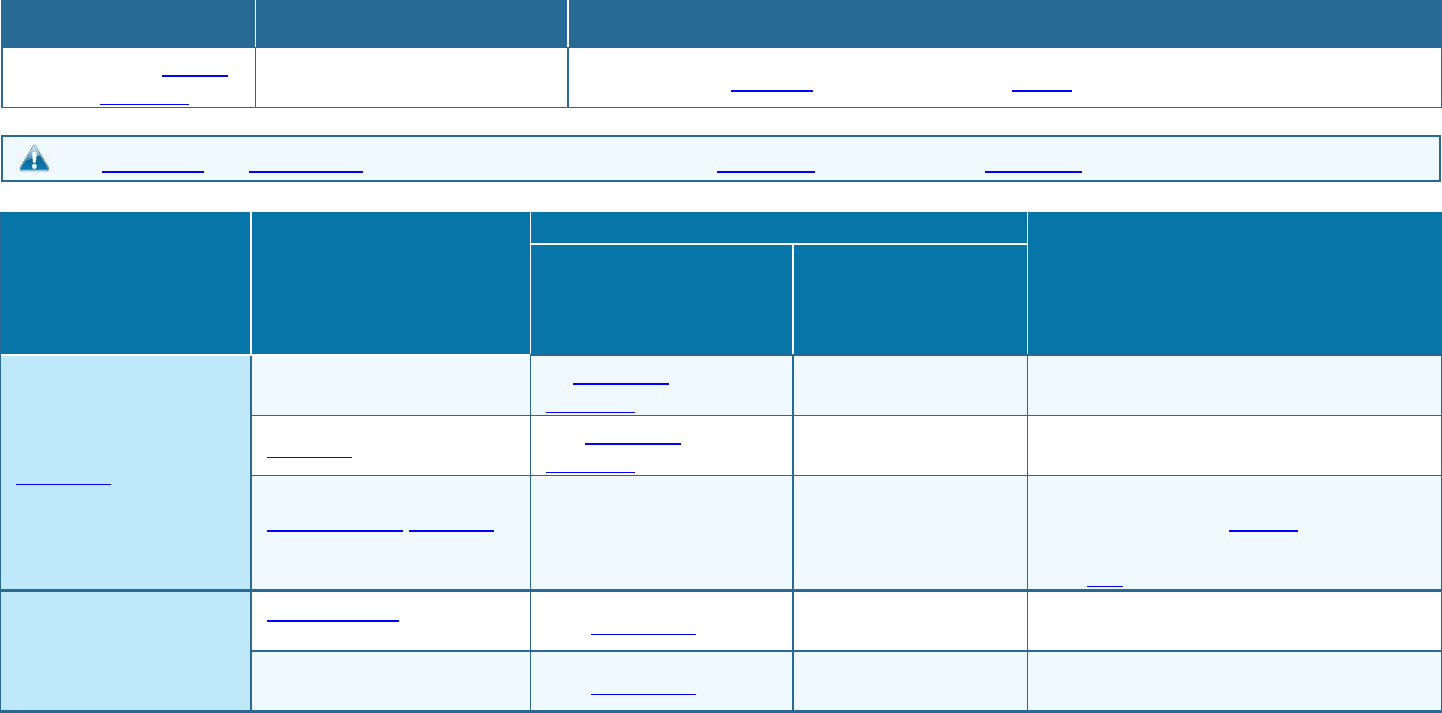
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.
Common Medical Event
Services You May Need
What You Will Pay
Limitations, Exceptions, & Other
Important Information
Network Provider
(You will pay the least)
Out-of-Network
Provider
(You will pay the
most)
If you visit a health care
provider’s office or
clinic
Primary care visit to treat an
injury or illness
$0 copayment/visit;
deductible does not apply.
Not covered.
Refer to the policy for more information
about Virtual Care Services.
Specialist visit
$90 copayment/visit;
deductible does not apply.
Not covered.
None.
Preventive care/screening/
immunization
No charge.
Not covered.
You may have to pay for services that aren’t
preventive. Ask your provider if the services
needed are preventive. Then check what
your plan will pay.
If you have a test
Diagnostic test (x-ray, blood
work)
25% coinsurance
Not covered.
None.
Imaging (CT/PET scans,
MRIs)
25% coinsurance
Not covered.
None.
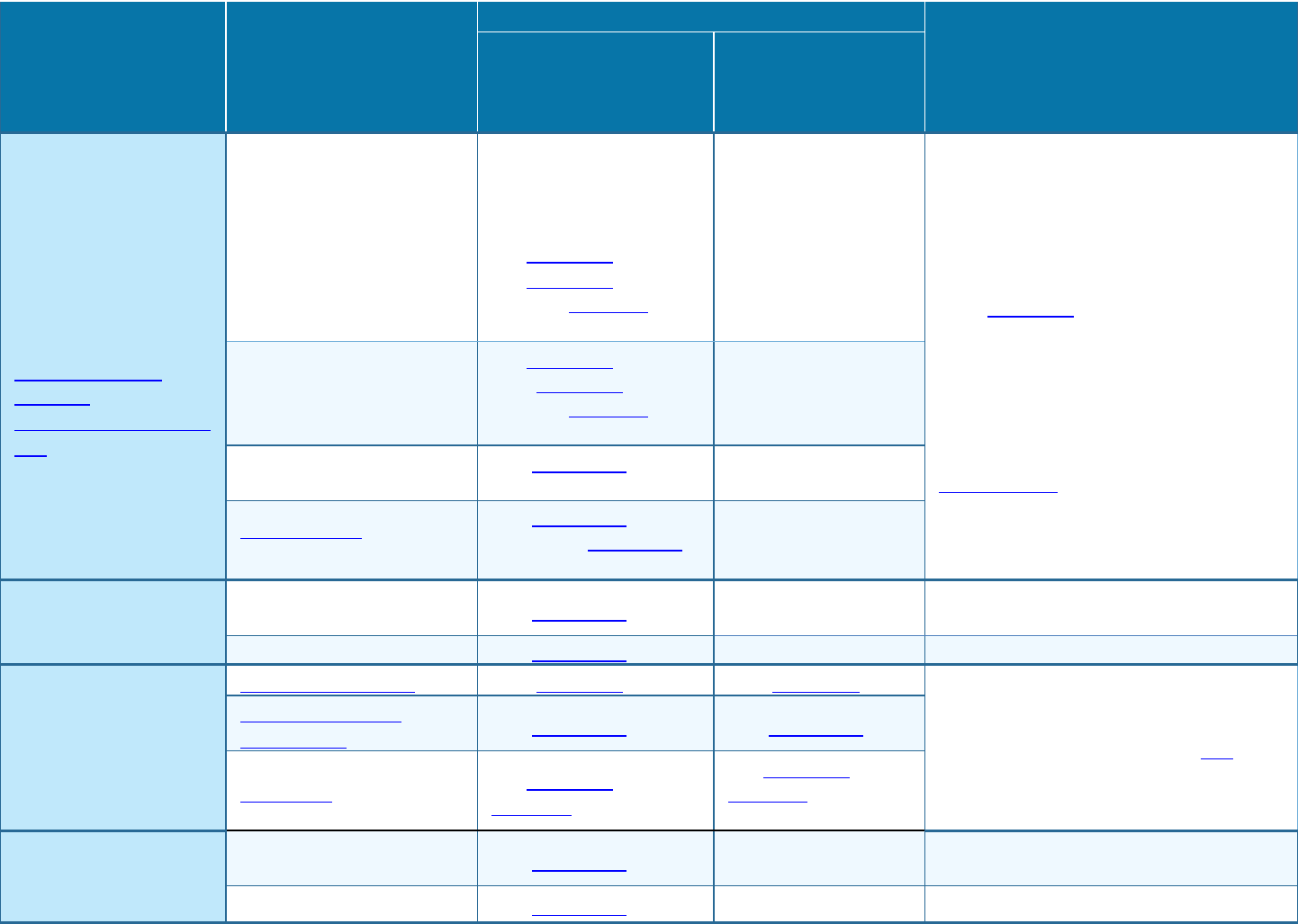
Page 3 of 6
Common Medical Event
Services You May Need
What You Will Pay
Limitations, Exceptions, & Other
Important Information
Network Provider
(You will pay the least)
Out-of-Network
Provider
(You will pay the
most)
If you need drugs to
treat your illness or
condition
More information about
prescription drug
coverage is available at
www.cigna.com/ifp-drug-
lists
Generic drugs
Preventive drugs:
No charge (retail/home
delivery).
Generic:
$20 copayment (retail)/
$60 copayment (home
delivery); deductible does
not apply.
Not covered.
Generic, Preferred, and Non-Preferred
Drugs: Limited to up to a 30-day supply
(retail) or a 90-day supply (Designated 90-
day retail pharmacy/home delivery). You
pay a copayment for each 30-day supply
(retail), if applicable.
Specialty Drugs: Limited to up to a 30-day
supply (retail) or a 30-day supply
(Designated 90-day retail pharmacy/home
delivery). Cigna Healthcare’s specialty
pharmacy can assist you in obtaining your
specialty drugs. Call Accredo, at
877.826.7657 to talk to a representative.
Preferred brand drugs
$90 copayment (retail)/
$270 copayment (home
delivery); deductible does
not apply.
Not covered.
Non-preferred drugs
50% coinsurance
(retail/home delivery)
Not covered.
Specialty drugs and other
high cost drugs
50% coinsurance
(retail)/40% coinsurance
(home delivery)
Not covered.
If you have outpatient
surgery
Facility fee (e.g., ambulatory
surgery center)
25% coinsurance
Not covered.
None.
Physician/surgeon fees
25% coinsurance
Not covered.
None.
If you need immediate
medical attention
Emergency room care
$600 copayment/visit.
$600 copayment/visit.
You pay the same level as In-network if it is
an emergency as defined in your plan,
otherwise Not covered.
Emergency medical
transportation
25% coinsurance
25% coinsurance
Urgent care
$50 copayment/visit;
deductible does not apply.
$50 copayment/visit;
deductible does not
apply.
If you have a hospital
stay
Facility fee (e.g., hospital
room)
25% coinsurance
Not covered.
None.
Physician/surgeon fees
25% coinsurance
Not covered.
None.
Page 4 of 6
Common Medical Event
Services You May Need
What You Will Pay
Limitations, Exceptions, & Other
Important Information
Network Provider
(You will pay the least)
Out-of-Network
Provider
(You will pay the
most)
If you need mental
health, behavioral
health, or substance
abuse services
Outpatient services
Office Visit: 25%
coinsurance; deductible
does not apply. All other
outpatient services: 25%
coinsurance.
Not covered.
Includes medical services for MH/SA
diagnoses.
Inpatient services
25% coinsurance
Not covered.
Includes medical services for MH/SA
diagnoses.
If you are pregnant
Office visits
25% coinsurance
Not covered.
Cost sharing does not apply for preventive
services. Depending on the type of services,
coinsurance may apply. Maternity care may
include tests and services described
elsewhere in the SBC (i.e. ultrasound).
Childbirth/delivery
professional services
25% coinsurance
Not covered.
Childbirth/delivery facility
services
25% coinsurance
Not covered.
If you need help
recovering or have
other special health
needs
Home health care
25% coinsurance
Not covered.
Coverage is limited to 28 hours per week.
Rehabilitation services
$0 copayment /visit for
physical and occupational
therapy; deductible does
not apply; 25%
coinsurance for all other
services.
Not covered.
Speech Therapy is limited to 20 visits
annual max.
Habilitation services
25% coinsurance
Not covered.
Coverage is limited to 20 visits annual max
per therapy.
Skilled nursing care
25% coinsurance
Not covered.
Coverage is limited to 100 days annual max.
Durable medical equipment
25% coinsurance
Not covered.
None.
Hospice services
25% coinsurance
Not covered.
None.
If your child needs
dental or eye care
Children’s eye exam
No charge.
Not covered.
Children up to age 19. Coverage limited to
one exam/year.
Children’s glasses
No charge.
Not covered.
Children up to age 19. Coverage limited to
one pair of glasses (lenses and frames from
pediatric selection), per every two years.
Children’s dental check-up
Not covered.
Not covered.
Coverage is available through a stand-alone
dental policy.
Page 5 of 6
Excluded Services & Other Covered Services:
Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.)
• Abortion (except in cases of rape, incest, or
when the life of the mother is endangered)
• Cosmetic surgery
• Dental care (Adult)
• Dental care (Child) (coverage available through
a stand-alone dental policy)
• Long-term care
• Non-emergency care when traveling outside the
U.S.
• Routine eye care (Adult)
• Routine foot care
• Weight loss programs
Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.)
• Acupuncture (unlimited visits annual max)
• Bariatric surgery
• Chiropractic care (unlimited visits annual max)
• Hearing aids (limited to 1 hearing aid per ear
every 3 years, to age 18)
• Infertility Treatment
• Private-duty nursing
Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those
agencies is: Colorado Department of Insurance at 1-800-930-3745. Other coverage options may be available to you, too, including buying individual insurance
coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318-2596. For more
information on your rights to continue coverage, contact the insurer at 1-866-494-2111.
Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called a
grievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents also
provide complete information on how to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or
assistance, contact: Colorado Department of Insurance at 1-800-930-3745.
Does this plan provide Minimum Essential Coverage? Yes.
Minimum Essential Coverage generally includes plans, health insurance available through the Marketplace or other individual market policies, Medicare, Medicaid,
CHIP, TRICARE, and certain other coverage. If you are eligible for certain types of Minimum Essential Coverage, you may not be eligible for the premium tax credit.
Does this plan meet the Minimum Value Standards? Not Applicable.
Language Access Services:
Spanish (Español): Para obtener asistencia en Español, llame al 1-866-494-2111.
Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 1-866-494-2111.
Chinese (中文): 如果需要中文的帮助,请拨打这个号码1-866-494-2111.
Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' 1-866-494-2111.
To see examples of how this plan might cover costs for a sample medical situation, see the next section.
Page 6 of 6
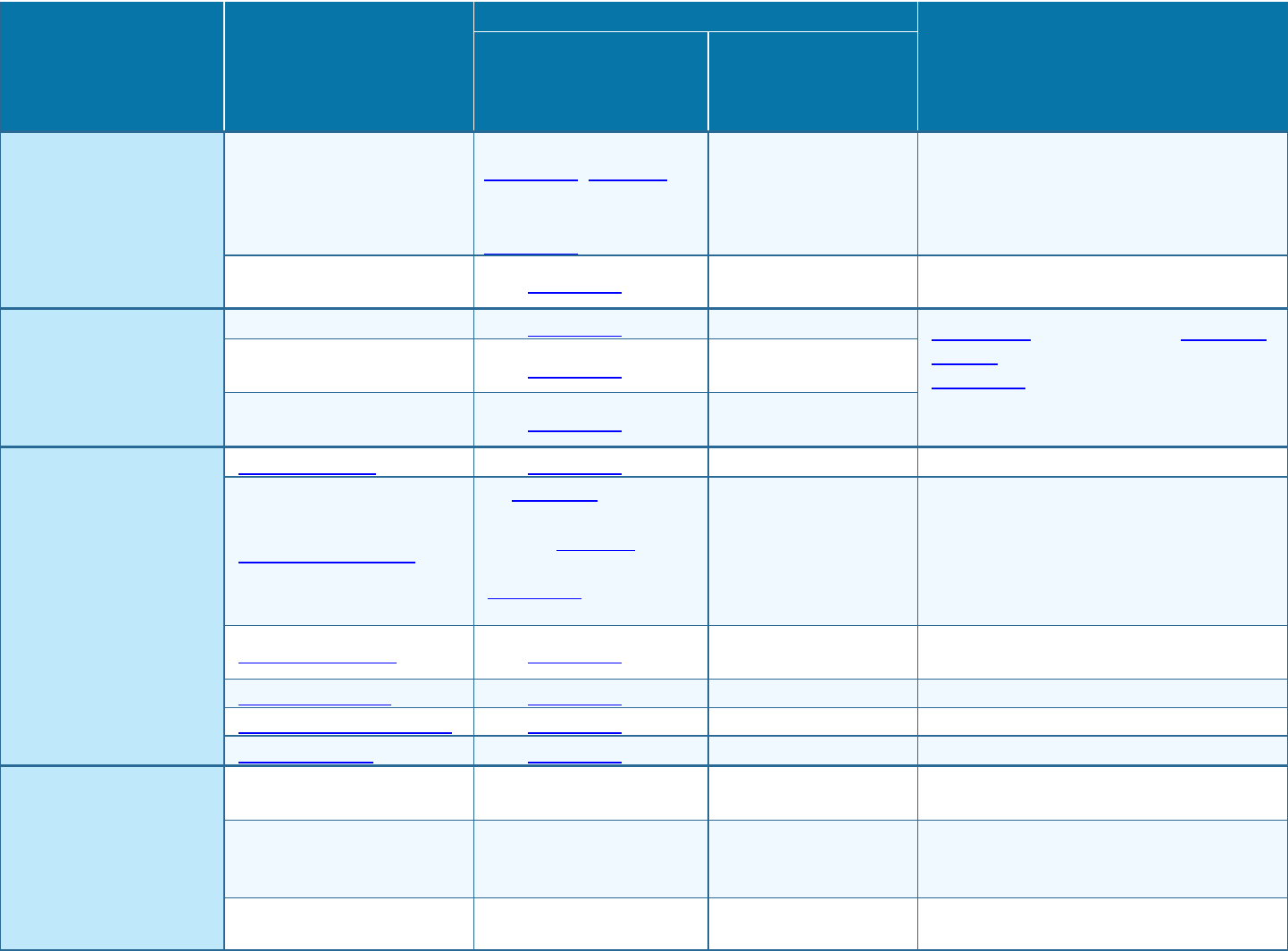
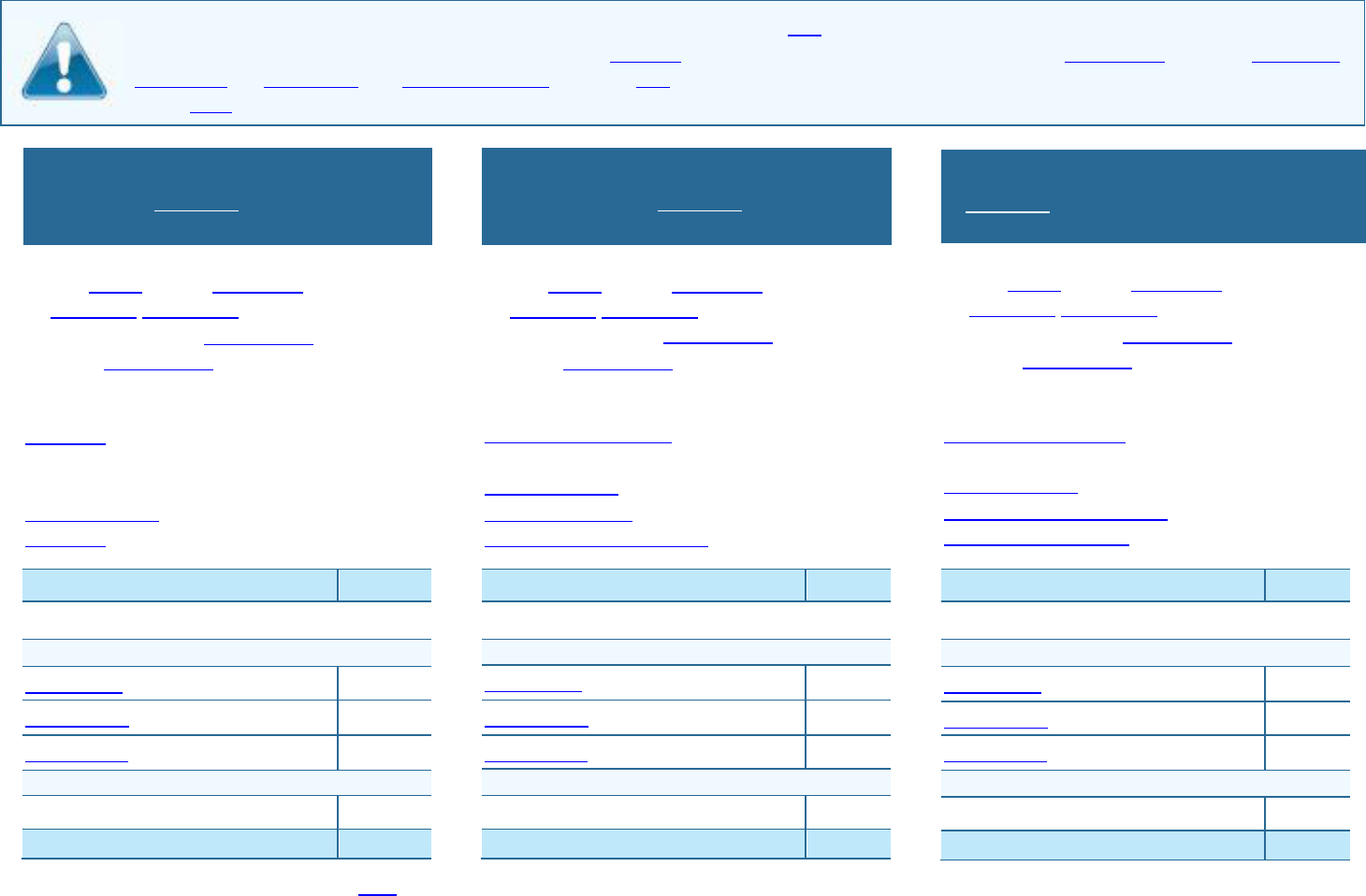
About these Coverage Examples:
This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different
depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost-sharing amounts (deductibles,
copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you might pay under different
health plans. Please note these coverage examples are based on self-only coverage.
◼ The plan’s overall deductible $4,000
◼ Specialist copayment $90
◼ Hospital (facility) coinsurance 25%
◼ Other coinsurance 25%
This EXAMPLE event includes services like:
Specialist office visits (prenatal care)
Childbirth/Delivery Professional Services
Childbirth/Delivery Facility Services
Diagnostic tests (ultrasounds and blood work)
Specialist visit (anesthesia)
Total Example Cost
$12,700
In this example, Peg would pay:
Cost Sharing
Deductibles
$4,000
Copayments
$10
Coinsurance
$2,100
What isn’t covered
Limits or exclusions
$60
The total Peg would pay is
$6,170
◼ The plan’s overall deductible $4,000
◼ Specialist copayment $90
◼ Hospital (facility) coinsurance 25%
◼ Other coinsurance 25%
This EXAMPLE event includes services like:
Primary care physician office visits (including
disease education)
Diagnostic tests (blood work)
Prescription drugs
Durable medical equipment (glucose meter)
Total Example Cost
$5,600
In this example, Joe would pay:
Cost Sharing
Deductibles
$900
Copayments
$600
Coinsurance
$0
What isn’t covered
Limits or exclusions
$20
The total Joe would pay is
$1,520
◼ The plan’s overall deductible $4,000
◼ Specialist copayment $90
◼ Hospital (facility) coinsurance 25%
◼ Other coinsurance 25%
This EXAMPLE event includes services like:
Emergency room care (including medical
supplies)
Diagnostic tests (x-ray)
Durable medical equipment (crutches)
Rehabilitation services (physical therapy)
Total Example Cost
$2,800
In this example, Mia would pay:
Cost Sharing
Deductibles
$1,700
Copayments
$300
Coinsurance
$0
What isn’t covered
Limits or exclusions
$0
The total Mia would pay is
$2,000
The plan would be responsible for the other costs of these EXAMPLE covered services.
Mia’s Simple Fracture
(in-network emergency room visit and follow up
care)
Managing Joe’s Type 2 Diabetes
(a year of routine in-network care of a well-
controlled condition)
Peg is Having a Baby
(9 months of in-network pre-natal care and a
hospital delivery)
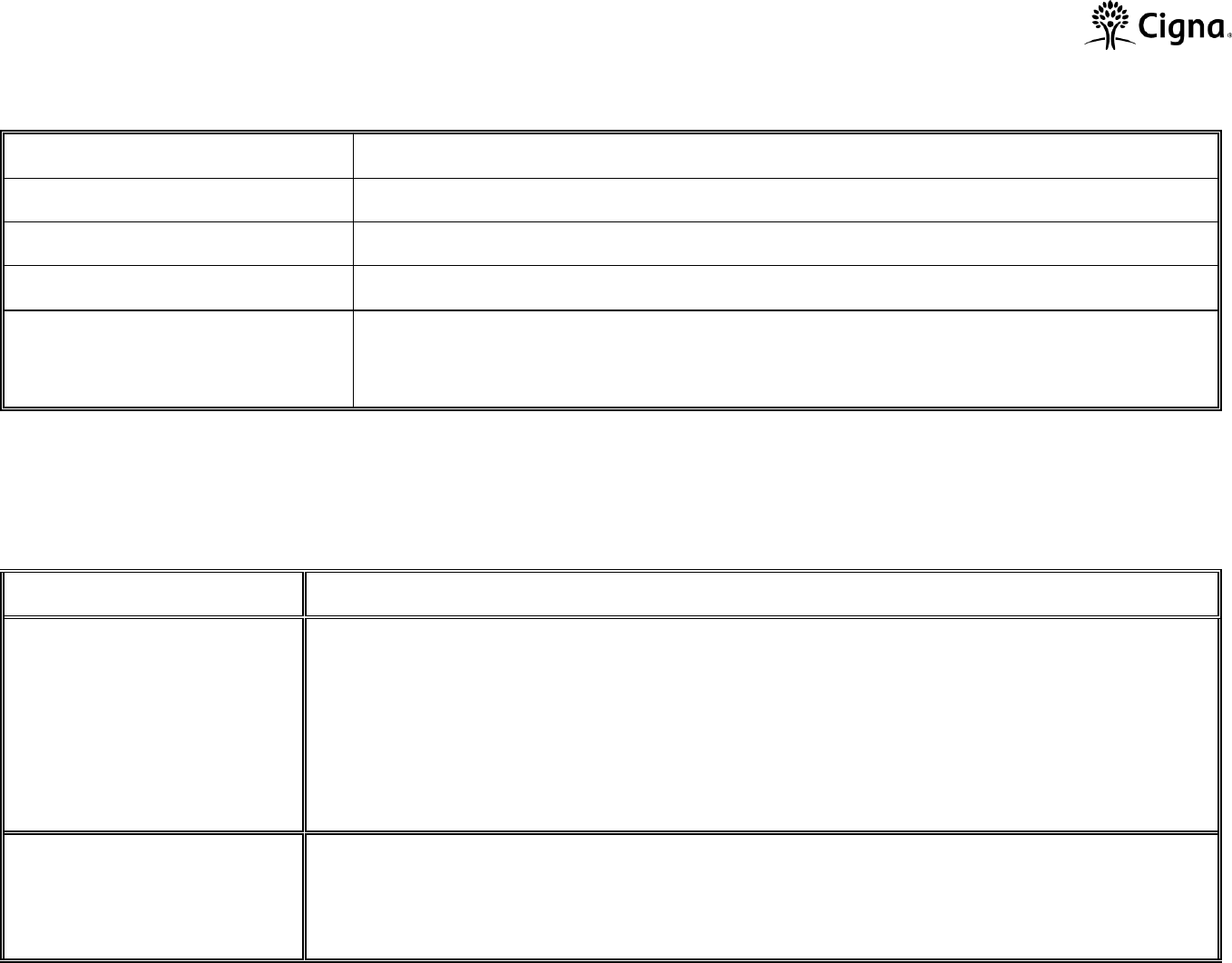
Colorado Supplement to the Summary of Benefits and Coverage Form
INSURANCE COMPANY NAME
Cigna Health and Life Insurance Company
NAME OF PLAN
Cigna Connect Flex Silver 5750
1. Type of Policy
Individual Policy
2. Type of plan
Exclusive provider organization (EPO)
3. Areas of Colorado where plan is
available.
Plan is available only in the following areas: Adams, Arapahoe, Boulder, Broomfield, Denver, Douglas,
El Paso, Jefferson, Larimer, Teller, Weld
SUPPLEMENTAL INFORMATION REGARDING BENEFITS
Important Note: The contents of this form are subject to the provisions of the policy, which contains all terms, covenants and conditions of coverage. It
provides additional information meant to supplement the Summary of Benefits of Coverage you have received for this plan. This plan may exclude
coverage for certain treatments, diagnoses, or services not specifically noted. Consult the actual policy to determine the exact terms and conditions of
coverage.
Description
4. Annual Deductible Type
EMBEDDED DEDUCTIBLE
INDIVIDUAL – The amount that each member of the family must meet prior to claims being paid. Claims will
not be paid for any other individual until their individual deductible or the family deductible has been met.
FAMILY – The maximum amount that the family will pay for the year. The family deductible can be met by
any number of individuals.
5. Out-of-Pocket Maximum
EMBEDDED OUT-OF-POCKET
INDIVIDUAL – The amount that each member of the family must meet prior to claims being paid at 100%.
Claims will not be paid at 100% for any other individual until their individual out-of-pocket or the family out-of-
pocket has been met.
FAMILY – The maximum amount that the family will pay for the year. The family out-of-pocket can be met by
any number of individuals.
6. What is included in the In-
Network Out-of-Pocket
Maximum?
Deductibles, Copayments and Coinsurance
7. Is pediatric dental covered
by this plan?
No, the plan does not include pediatric dental
8. What cancer screenings
are covered?
Breast Cancer Screening with Mammography, Cervical Cancer Screening, Colorectal Cancer Screening,
Prostate Cancer Screening
USING THE PLAN
IN-NETWORK
OUT-OF-NETWORK
9. If the provider charges more for a covered service than the plan
normally pays, does the enrollee have to pay the difference?
No
N/A
10. Does the plan have a binding arbitration clause?
No
Questions: Call 1-800-244-6224 or visit us at www.cigna.com.
ATENCIÓN: tiene a su disposición servicios gratuitos de asistencia lingüística. Si es un cliente actualde Cigna, llame al número que figura en el reverso
de su tarjeta de identificación. Si no lo es, llame al 1-800-244-6224 (los usuarios de TTY deben llamar al 711).
If you are not satisfied with the resolution of your complaint or grievance, contact: Colorado Division of Insurance
Consumer Services, Life and Health Section
1560 Broadway, Suite 850, Denver, CO 80202
Call: 303-894-7490 (in-state, toll-free: 800-930-3745)
Email: dora_insurance@state.co.us

Cigna Healthcare complies with applicable
Federal civil rights laws and does not
discriminate on the basis of race, color, national
origin, age, disability, sex, gender identity or
sexual orientation. Cigna Healthcare does not
exclude people or treat them differently because
of race, color, national origin, age, disability, sex,
gender identity or sexual orientation.
– Qualified sign language interpreters
– Written information in other formats (large
print, audio, accessible electronic formats,
other formats)
– Qualified interpreters
– Information written in other languages
If you need these services, contact customer
service at the toll-free number shown on your ID
card, and ask a Customer Service Associate for
assistance.
If you believe that Cigna Healthcare has failed to
provide these services or discriminated in another
way on the basis of race, color, national origin,
age, disability, or sex, you can file a grievance by
sending an email to [email protected] or
by writing to the following address:
Cigna Healthcare
Nondiscrimination Complaint Coordinator
P.O. Box 188016 Chattanooga, TN 37422
If you need assistance filing a written grievance,
please call the number on the back of your ID card
or send an email to ACAGrievance@Cigna.com.
You can also file a civil rights complaint with the U.S.
Department of Health and Human Services, Office
for Civil Rights electronically through the Office for
Civil Rights Complaint Portal, available at
https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by
mail or phone at:
U.S. Department of Health and Human Services
200 Independence Avenue, SW
Room 509F, HHH Building
Washington, DC 20201
1.800.368.1019, 800.537.7697 (TDD)
Complaint forms are available at
http://www.hhs.gov/ocr/office/file/index.html
Discrimination is against the law.
Medical coverage
Proficiency of Language Assistance Services
English – ATTENTION: Language assistance services, free of charge, are available to you. For current Cigna
customers, call the number on the back of your ID card. Otherwise, call 1.800.244.6224 (TTY: Dial 711).
Spanish – ATENCIÓN: Hay servicios de asistencia de idiomas, sin cargo, a su disposición. Si es un cliente
actual de Cigna, llame al número que figura en el reverso de su tarjeta de identificación. Si no lo es, llame
al 1.800.244.6224 (los usuarios de TTY deben llamar al 711).
Chinese – 注意:我們可為您免費提供語言協助服務。對於 Cigna 的現有客戶,請致電您的 ID 卡背面的號碼。其
他客戶請致電 1.800.244.6224 (聽障專線:請撥 711)。
Vietnamese
Korean – 주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무료로 이용하실 수 있습니다. 현재 Cigna
가입자님들께서는 ID 카드 뒷면에 있는 전화번호로 연락해주십시오. 기타 다른 경우에는 1.800.244.6224
(TTY: 다이얼 711)번으로 전화해주십시오.
Tagalog – PAUNAWA: Makakakuha ka ng mga serbisyo sa tulong sa wika nang libre. Para sa mga
kasalukuyang customer ng Cigna, tawagan ang numero sa likuran ng iyong ID card. O kaya, tumawag sa
1.800.244.6224 (TTY: I-dial ang 711).
Russian
Cigna – Arabic
711:TTY) 1.800.244.6224
French Creole – ATANSYON: Gen sèvis èd nan lang ki disponib gratis pou ou. Pou kliyan Cigna yo, rele
nimewo ki dèyè kat ID ou. Sinon, rele nimewo 1.800.244.6224 (TTY: Rele 711).
French – ATTENTION : Des services d’aide linguistique vous sont proposés gratuitement. Si vous êtes un
client actuel de Cigna, veuillez appeler le numéro indiqué au verso de votre carte d’identité. Sinon, veuillez
appeler le numéro 1.800.244.6224 (ATS: composez le numéro 711).
Portuguese – ATENÇÃO: Tem ao seu dispor serviços de assistência linguística, totalmente gratuitos. Para
clientes Cigna atuais, ligue para o número que se encontra no verso do seu cartão de identificação. Caso
contrário, ligue para 1.800.244.6224 (Dispositivos TTY: marque 711).
Polish – UWAGA: w celu skorzystania z dostępnej, bezpłatnej pomocy językowej, obecni klienci firmy
Cigna mogą dzwonić pod numer podany na odwrocie karty identyfikacyjnej. Wszystkie inne osoby
prosimy o skorzystanie z numeru 1 800 244 6224 (TTY: wybierz 711).
Japanese – 注意事項:日本語を話される場合、無料の言語支援サービスをご利用いただけます。現在のCignaの
お客様は、IDカード裏面の電話番号まで、お電話にてご連絡ください。その他の方は、1.800.244.6224(TTY: 711)
まで、お電話にてご連絡ください。
Italian – ATTENZIONE: Sono disponibili servizi di assistenza linguistica gratuiti. Per i clienti Cigna attuali,
chiamare il numero sul retro della tessera tessera di identificazione. In caso contrario, chiamare il numero
1.800.244.6224 (utenti TTY: chiamare il numero 711).
German – ACHTUNG: Die Leistungen der Sprachunterstützung stehen Ihnen kostenlos zur Verfügung.
Wenn Sie gegenwärtiger Cigna-Kunde sind, rufen Sie bitte die Nummer auf der Rückseite Ihrer
Krankenversicherungskarte an. Andernfalls rufen Sie 1.800.244.6224 an (TTY: Wählen Sie 711).
Cigna– Persian (Farsi)
711
1.800.244.6224
824707 5/23
