Page 1 of 13
Medical Coverage Policy: 0152
Medical Coverage Policy
Effective Date .................... 8/15/2024
Next Review Date .............. 8/15/2025
Coverage Policy Number ............. 0152
Breast Reduction
Table of Contents
Overview ............................................ 2
Coverage Policy .................................... 2
Health Equity Considerations .................. 3
General Background ............................. 3
Medicare Coverage Determinations ......... 7
Appendix ............................................. 7
Coding Information ............................... 8
References .......................................... 9
Revision Details ................................. 12
Related Coverage Resources
Acupuncture
Breast Reconstruction following Mastectomy or
Lumpectomy
Chiropractic Care
Complementary and Alternative Medicine
Physical Therapy
Gynecomastia Surgery
Gender Dysphoria Treatment
INSTRUCTIONS FOR USE
The following Coverage Policy applies to health benefit plans administered by Cigna Companies.
Certain Cigna Companies and/or lines of business only provide utilization review services to clients
and do not make coverage determinations. References to standard benefit plan language and
coverage determinations do not apply to those clients. Coverage Policies are intended to provide
guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please
note, the terms of a customer’s particular benefit plan document [Group Service Agreement,
Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan
document] may differ significantly from the standard benefit plans upon which these Coverage
Policies are based. For example, a customer’s benefit plan document may contain a specific
exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s
benefit plan document always supersedes the information in the Coverage Policies. In the absence
of a controlling federal or state coverage mandate, benefits are ultimately determined by the
terms of the applicable benefit plan document. Coverage determinations in each specific instance
require consideration of 1) the terms of the applicable benefit plan document in effect on the date
of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including
Coverage Policies and; 4) the specific facts of the particular situation. Each coverage request
should be reviewed on its own merits. Medical directors are expected to exercise clinical judgment
where appropriate and have discretion in making individual coverage determinations. Where
coverage for care or services does not depend on specific circumstances, reimbursement will only
be provided if a requested service(s) is submitted in accordance with the relevant criteria outlined
in the applicable Coverage Policy, including covered diagnosis and/or procedure code(s).
Reimbursement is not allowed for services when billed for conditions or diagnoses that are not
covered under this Coverage Policy (see “Coding Information” below). When billing, providers
must use the most appropriate codes as of the effective date of the submission. Claims submitted

Page 2 of 13
Medical Coverage Policy: 0152
for services that are not accompanied by covered code(s) under the applicable Coverage Policy
will be denied as not covered. Coverage Policies relate exclusively to the administration of health
benefit plans. Coverage Policies are not recommendations for treatment and should never be used
as treatment guidelines. In certain markets, delegated vendor guidelines may be used to support
medical necessity and other coverage determinations.
Overview
This Coverage Policy addresses breast reduction for symptomatic macromastia and breast
reduction surgery on the nondiseased/contralateral breast following a mastectomy or lumpectomy.
Coverage Policy
Coverage for breast reduction varies across plans. Please refer to the customer’s benefit
plan document for coverage details.
Breast reduction surgery on the nondiseased/contralateral breast when performed to
produce a symmetrical appearance following a mastectomy or lumpectomy is
considered medically necessary.
If coverage for breast reduction is available, the following conditions of coverage apply.
Breast reduction is considered medically necessary for the treatment of macromastia
(i.e., large breasts) in women at least 18 years of age, or with completed breast growth,
when ALL the following criteria are met:
• macromastia is causing at least ONE of the following conditions/symptoms that has been
unresponsive to medical management:
shoulder, upper back/ neck pain, and/or ulnar nerve palsy for which no other
etiology has been found on appropriate evaluation
intertrigo, dermatitis, eczema, or hidradenitis at the inframammary fold
• preoperative photographs confirm the presence of:
significant breast hypertrophy
shoulder grooving from bra straps and/or intertrigo (if stated to be present)
• average grams of tissue to be removed per breast are above the 22nd percentile on the
Schnur Sliding Scale (see Appendix A) based on the individual's body surface area (BSA) or
regardless of BSA, more than 1 kg of breast tissue will be removed per breast
Breast reduction or mastopexy prior to mastectomy is considered medically necessary
when a staged procedure is planned prior to a nipple-sparing mastectomy.
Note: The following are considered integral to breast reduction (CPT
®
code 19318) and
not separately reimbursable:
• Nipple and areola reconstruction (CPT
®
code 19350)
• Suction lipectomy or ultrasonically-assisted suction lipectomy (liposuction) (CPT
®
code 15877)
Breast reduction for either of the following indications is considered cosmetic in nature
and not medically necessary:

Page 3 of 13
Medical Coverage Policy: 0152
• surgery is being performed to treat psychological symptomatology or psychosocial
complaints, in the absence of significant physical findings that meet the above listed
criteria
• surgery is being performed for the sole purpose of improving appearance
Correction of benign inverted nipples (CPT
®
code 19355) is considered cosmetic in
nature and not medically necessary.
Suction lipectomy or ultrasonically-assisted suction lipectomy (liposuction) as a sole
method of treatment for symptomatic macromastia is considered unproven.
Health Equity Considerations
Health equity is the highest level of health for all people; health inequity is the avoidable
difference in health status or distribution of health resources due to the social conditions in which
people are born, grow, live, work, and age.
Social determinants of health are the conditions in the environment that affect a wide range of
health, functioning, and quality of life outcomes and risks. Examples include safe housing,
transportation, and neighborhoods; racism, discrimination and violence; education, job
opportunities and income; access to nutritious foods and physical activity opportunities; access to
clean air and water; and language and literacy skills.
Sociodemographic and economic disparities have a role in outcomes related to breast reduction.
In a retrospective observational study of 414 women who underwent inpatient bilateral reduction
mamamoplasty, comorbidity, age, race, payor status and rural- urban density were evaluated for
risk of post op complications. Higher comorbidity index (p<0.001), Black race (p<0.001) and
treatment within a nonmetropolitan or rural county (p=0.0017) were significant predictors of
increased risk of postoperative complication. Age, comorbidity severity, race and zip code income
quartile were also evaluated for risk of extended length of stay. Older age (p= 0.0078), increased
comorbidity severity (p< 0.001) and Black race (p= 0.0011) predicted higher risk of extended
length of stay, whereas Hispanic race predicted decrease of such risk (p< 0.001) (Kim and
Ascherman, 2024).
General Background
Macromastia (i.e., female breast hypertrophy) is the development of abnormally large breasts.
Normal breast development begins at approximately five weeks’ gestation and continues until a
woman is in her early twenties, with the rate of development and degree of asymmetry often
varying. Spontaneous massive growth of the breasts during puberty and adolescence is thought to
be the result of excessive end-organ sensitivity to gonadal hormones. It is more commonly
bilateral, often occurs over a brief period, and most commonly affects adolescent girls.
Management is individualized and may range from reassurance or the use of supportive
brassieres. It is recommended that surgery be delayed until late adolescence to allow complete
breast development (Conner and Merritt, 2020; McGrath and Pomerantz, 2012).
The presence of macromastia may cause clinical manifestations when the excessive breast weight
adversely affects the supporting structures of the shoulders, neck, and trunk. Increased weight on
the shoulders can cause pain, fatigue in the cervical and thoracic spine, which can lead to poor
posture, thoracic kyphosis and occipital headaches. Grooving or ulceration of the skin on the
shoulders, pressure on the brachial plexus causing neurological symptoms in the arms and skin
conditions occurring at the inframammary fold such as intertrigo, dermatitis, eczema, or
Page 4 of 13
Medical Coverage Policy: 0152
hidradenitis (inflammation of the apocrine sweat glands resulting in obstruction of the ducts) may
also exist. The presence of these persistent signs and painful symptoms distinguishes
macromastia from large, normal breasts and may prompt the need for surgical intervention
(American Society of Plastic Surgeons [ASPS], 2011/2021; McGrath and Pomerantz, 2012;
Schnur, et al., 1997).
Medical management of conditions/symptoms may include any of the following: weight loss;
acupuncture; massage therapy; chiropractic treatment; adequate bra support (proper fit and wide
strap support); nonsteroidal anti-inflammatory drugs (NSAIDS)/analgesia; and physical therapy,
when a functional impairment exists (Hansen and Chang, 2023; Collins, et al., 2002).
Reduction mammoplasty is the surgical excision of a substantial portion of the breast, including
the skin and the underlying glandular tissue, until a clinically normal size is obtained. Relocation of
the nipple, which may result in decreased sensation and altered lactation, may also be required
during this procedure. Therefore, it has been recommended that surgery should not be performed
on an individual until the breasts are fully developed. Complications range from mild to severe and
may be early or late. The most common early complication independent of reduction technique is
delayed wound healing. Late complications can include, but are not limited to, seroma, scars and
pseudoptosis. A BMI ≥30 kg/m
2
and smoking may increase the risk of complications. Persons who
are obese or irradiated are more likely to develop infections, and smokers experienced a higher
incidence of wound dehiscence than did nonsmokers (Zhang, et al., 2016; McGrath and
Pomerantz, 2012; Nahai, et al., 2008; Greydanus, et al., 2006).
Amaral et al. (2011) reported on racial and socioeconomic disparities in reduction mammoplasty.
Their analysis of the 2007 Nationwide Inpatient Sample database for differences in race and payer
mix revealed that Black and Hispanic patients (p<0.0001) were more likely to undergo reduction
mammoplasty.
The available techniques for breast reduction differ according to the pattern of skin resection, as
well as the method for removing breast tissue and moving the nipple. Factors identified on the
preoperative breast evaluation that are used for determining the best approach include
preoperative breast size and degree of ptosis, desired postoperative breast size, skin quality, and
a history of prior breast surgery. Liposuction for conturing to remove excess fat in the lateral area
of the breast at the time of surgery is considered part of the breast reduction procedure (Pu,
2021; Cohen, 2018). Among these, preoperative breast size and estimated breast reduction
volume are the most important factors influencing the technique selected. Generally, breast
hypertrophy is stratified according to the estimated volume to be resected:
• small reductions remove 200 to 400 grams per side
• moderate reductions remove 400 to 700 grams per side
• large reductions remove 700 to 1200 grams per side
• reductions in patients with gigantomastia involve massive reductions of more than 1200
grams per side
Several methods are available to help surgeons estimate breast resection volumes. The two most
common methods are the Schnur sliding scale and the Descamps formula. The Schnur sliding
scale estimates resection weight based on the patient's body surface area. The Descamps method
estimates resection volume based on a regression analysis (Hansen and Chang, 2023). There is no
consensus on which formula to use to calculate body surface area (Redlarski, et. al., 2016).
The Schnur Sliding Scale is an evaluation tool that may be used to determine the appropriate
amount of tissue to be removed compared to a patient’s total body surface area (BSA). This can
be instrumental in determining if breast reduction is being planned for a purely cosmetic reason or
as a medically necessary procedure. In a survey of plastic surgeons, Schnur et al. (1991)
Page 5 of 13
Medical Coverage Policy: 0152
concluded that women whose removed breast weight was less than the 5th percentile sought the
procedure for cosmetic reasons and all women whose breast weight was greater than the 22nd
percentile sought the procedure for medical reasons. One way to calculate the BSA is: BSA (in m
2
)
= [height (cm)]
0.718
X [weight (kilograms [kg])]
0.427
X .007449.
Generally, most patients do not require hospitalization after breast reduction surgery. An
overnight stay with observation may be necessary for some women with medical comorbidities.
Patients who experience severe postoperative nausea and vomiting may require extended
observation or admission for intravenous fluid therapy and antiemetics (Hansen and Chang,
2023).
Breast tissue regrowth following initial breast reduction in adolescence has been reported
(Greydanus, et al., 2006). The growth of the female breast is generally described by five stages
referred to as Tanner stages or sexually maturity rating (SMR) stages. A number of clinical
correlations are noted with the SMR stages, including the timing of breast reduction at stage V
(i.e., mature stage) (DeSilva, et al., 2006). In a review of elective plastic surgical procedures in
adolescence, McGrath and Schooler (2004) stated “Breast development is variable but usually
plateaus at 15–16 years of age. Reduction mammoplasty is postponed until breast maturity is
reached. Occasionally, surgery is considered earlier when severe symptoms are encountered;
there is a risk of recurrent hypertrophy, however.” In general, breast maturity should have been
reached prior to considering breast reduction surgery.
Staged breast reduction in patients with large and ptotic breasts has been shown to decrease
rates of major flap necrosis before nipple-sparing mastectomy and preserve the viability of the
nipple. Classification of breast ptosis (Regnault, 1976) is based on the relationship of the nipple to
the inframammary fold (IMF). In mild, or Grade I ptosis, the nipple is situated within 1 cm of the
inframammary fold and is above the lower pole of the breast. In moderate, or Grade II ptosis, the
nipple is 1–3 cm below the inframammary fold but is still located above the lowest point of the
breast. In severe, or grade III ptosis, the nipple is more than 3 cm below the inframammary fold
and is situated at the lowest part of the breast. Studies are primarily in the form of case series
and retrospective reviews with small patient populations (Tondu, 2022; Economides et al., 2019;
Saliban et al., 2019; Gunnarsson et al., 2017; Spear et al., 2012). Spear et al. (2012) first
described the procedure in a case series of 15 patients (24 breasts) who underwent nipple-sparing
mastectomy after mastopexy or reduction. Complications occurred in four (17%) of the 24 breasts
including skin flap necrosis (n=2 breasts), minimal partial nipple-areola complex necrosis (n=3
breasts) and an expander explanted for infection related to skin flap necrosis (n=1 breast).
Successful nipple-sparing mastectomy and prior mastopexy or reduction (without residual effects
of the nipple-areola complex or skin flap necrosis) occurred in 14 patients (23 breasts, 96%).
Nipple inversion or retraction is when the nipple is pulled in and points inward instead of out. It
can affect one breast or both and can be acquired or congenital. The cause of acquired nipple
inversion can be due to benign or malignant causes. Congenital nipple inversion is usually bilateral
and is benign (Killelea and Sowden, 2024). Correction of nipple inversion is considered cosmetic in
nature and not medically indicated.
Literature Review
Controlled clinical studies assessing the effectiveness of surgical removal of modest amounts of
breast tissue in reducing neck, shoulder, and back pain and related disabilities in women are
lacking. Despite the lack of controlled studies, reduction mammoplasty has become the standard
of care for a subset of individuals with symptomatic macromastia. Evidence suggests that
calculating breast reduction in correlation to each patient’s body weight and height can have an
effect on reducing preoperative signs and persistent physical conditions. (Cunningham, et al.,
Page 6 of 13
Medical Coverage Policy: 0152
2005; Blomqvist, et al., 2004; Souto, et al., 2003; Collins, et al., 2002; Ayhan, et al., 2002;
Bruhlmann, et al., 1998).
Chadbourne et al. (2001) conducted a systematic review and meta-analysis of 29 studies of 4173
patients to determine whether reduction mammoplasty improves measurable outcomes in women
with breast hypertrophy. Experimental and observational studies were included; no randomized
controlled trials were found. Outcomes assessed were postoperative physical signs and symptoms
such as shoulder pain, shoulder (bra strap) grooving, and quality-of-life domains, such as physical
and psychological functioning, and were expressed primarily as risk differences. The mean body
mass index of the patients was 27.5 kg/m
2
in the observational studies and 29.6 kg/m
2
in the
experimental studies. The average tissue mass removed per breast was approximately 1400
grams. The authors concluded that reduction mammoplasty was associated with a statistically
significant improvement in physical signs and symptoms involving shoulder pain, shoulder
grooving, upper/lower back pain, neck pain, intertrigo, breast pain, headache, and pain/numbness
in the hands. The quality-of-life parameter of physical functioning was also statistically significant,
while psychological functioning was not significant. The evidence suggests that women undergoing
reduction mammoplasty for breast hypertrophy have significant postoperative improvement in
preoperative signs and symptoms, quality of life, or both.
Breast Reduction by Liposuction
Suction lipectomy or ultrasonically assisted suction lipectomy (liposuction) as a sole procedure has
been introduced as an alternative method in reducing breast size. The effectiveness of liposuction,
in terms of removing glandular breast tissue, rather than fatty tissue in the breast, remains to be
demonstrated. Evidence supporting the effects of this approach on patient outcomes has been
limited to retrospective/prospective uncontrolled studies and case series, and there are minimal
long-term data comparing this technique to the standard surgical approach (Moskovitz, et al.,
2007; Sadove, et al., 2005).
Professional Societies/Organizations
American College of Obstetricians and Gynecologists (ACOG): In a Committee Opinion
(2017, reaffirmed 2020), ACOG recognizes that breast reduction surgery in adolescents with large
breasts can relieve back, shoulder, and neck pain. Recommendations for timing of surgery include
postponing surgery until breast maturity is reached, waiting until there is stability in cup size over
6 months, and waiting until the age of 18 years. The committee states that the timing may be
reasonably determined by the severity of symptoms. It is also recommended that an assessment
of the adolescent’s emotional, physiologic, and physical maturity be conducted.
American Society of Plastic Surgeons (ASPS): In 2022, the American Society of Plastic
Surgeons convened a multidisciplinary work group consisting of members of the American Society
of Plastic Surgeons, the American Society of Breast Surgeons, the American Physical Therapy
Association, and a patient representative to revise the 2012 guidelines for reduction
mammaplasty. After evaluating the evidence-based literature, the work group made the following
recommendations with level of evidence and strength of recommendation (Perdikis, et al., 2022):
• post-menarche female patients presenting with breast hypertrophy should be offered
reduction mammaplasty surgery as first-line therapy over non-operative therapy based
solely on the presence of multiple symptoms rather than resection weight (high evidence
quality, strong recommendation)
• clinicians should counsel post-menarche patients with symptomatic breast hypertrophy
considering reduction mammaplasty that they may have a higher risk of complications if
they are older than 50 years old, have a body mass index greater than 35 kg/m
2
, or
require chronic corticosteroid use (all independent variables) (moderate evidence quality,
moderate recommendation)
Page 7 of 13
Medical Coverage Policy: 0152
The 2011 update (reaffirmed 2021) to the 2002 ASPS policy statement, insurance coverage
criteria for third-party payors for reduction mammaplasty, recommends that justification for
reduction mammaplasty should be based on the probability of relieving the clinical signs and
symptoms of macromastia, not the degree of breast hypertrophy present (cup size or amount of
tissue removed). Symptomatic breast hypertrophy is defined as a syndrome of persistent neck
and shoulder pain, painful shoulder grooving from brassiere straps, chronic intertriginous rash of
the inframammary fold, and frequent episodes of headache, backache, and neuropathies caused
by heavy breasts caused by an increase in the volume and weight of breast tissue beyond normal
proportions. These policy recommendations are based on the 2011 ASPS evidence-based
companion guideline for Reduction Mammaplasty.
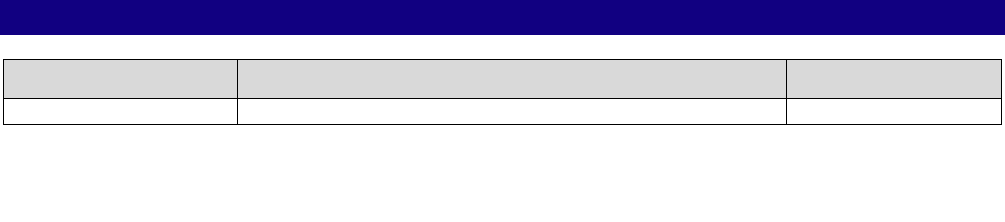
Medicare Coverage Determinations
Contractor
Determination Name/Number
Revision Effective
Date
NCD
National
No Determination found
LCD
National Government
Services, Inc.
Reduction Mammaplasty/L35001
11/07/2019
LCD
Noridian
Plastic Surgery/L35163 and L37020
10/01/2019
Note: Please review the current Medicare Policy for the most up-to-date information.
(NCD = National Coverage Determination; LCD = Local Coverage Determination)
Appendix
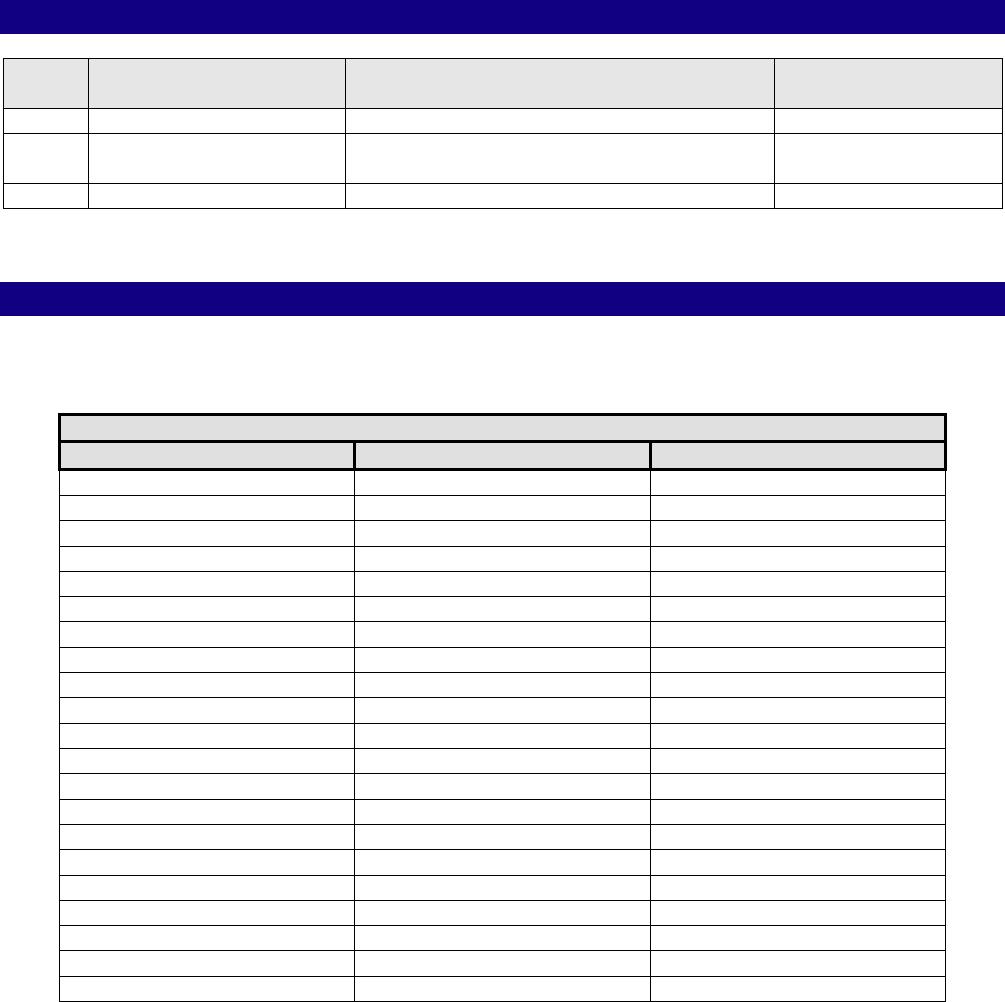
Schnur Sliding Scale
Body Surface Area and Cutoff Weight of Breast Tissue Removed
Breast Reduction (gm)
Body Surface Area (m
2
)
Lower 5%
Lower 22%
1.35
127
199
1.40
139
218
1.45
152
238
1.50
166
260
1.55
181
284
1.60
198
310
1.65
216
338
1.70
236
370
1.75
258
404
1.80
282
441
1.85
308
482
1.90
336
527
1.95
367
575
2.00
401
628
2.05
439
687
2.10
479
750
2.15
523
819
2.20
572
895
2.25
625
978
2.30
682
1068
2.35
745
1167
Page 8 of 13
Medical Coverage Policy: 0152
Breast Reduction (gm)
Body Surface Area (m
2
)
Lower 5%
Lower 22%
2.40
814
1275
2.45
890
1393
2.50
972
1522
2.55
1062
1662
Schnur Sliding Scale (Schnur, et al., 1991)
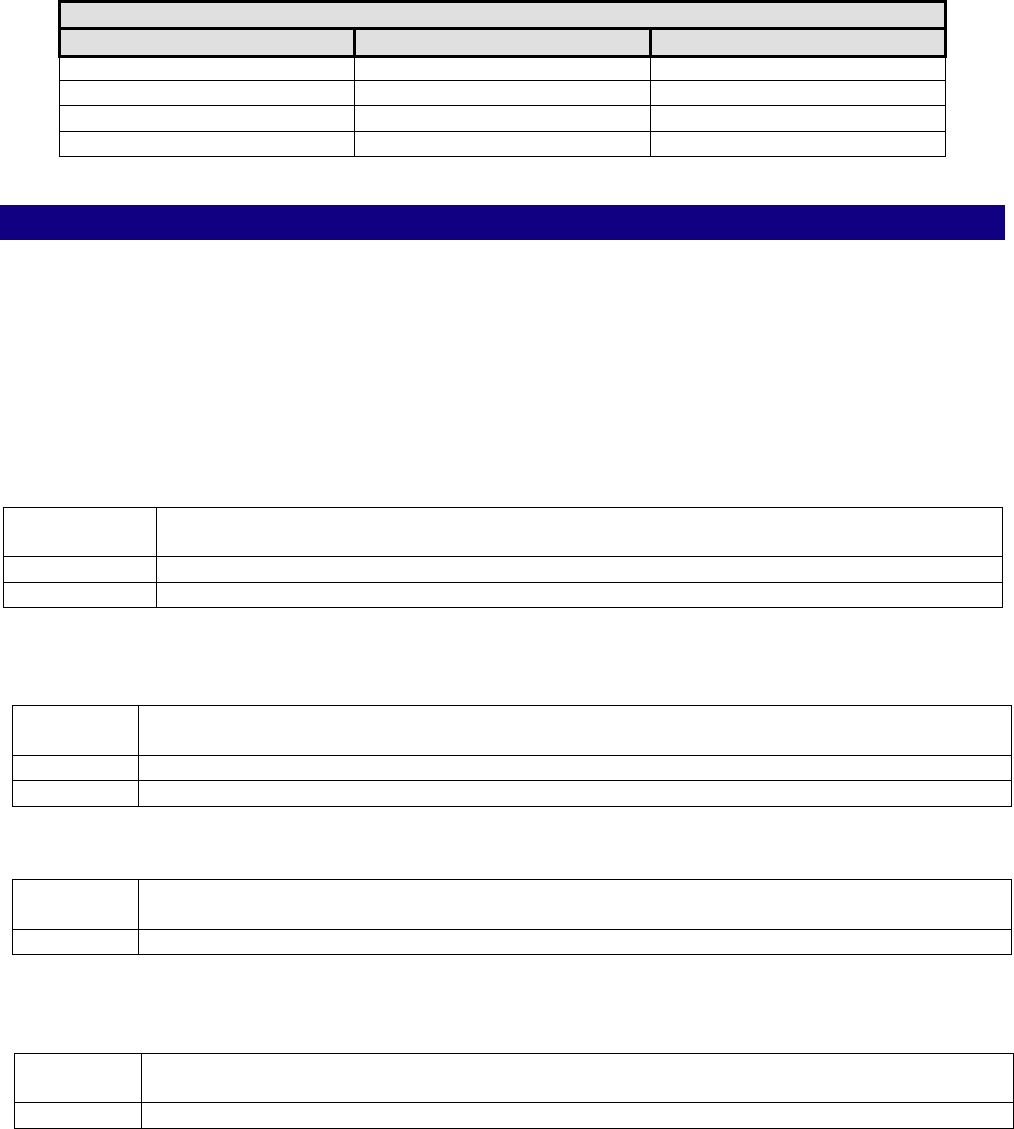
Coding Information
Notes:
1. This list of codes may not be all-inclusive since the American Medical Association (AMA)
and Centers for Medicare & Medicaid Services (CMS) code updates may occur more
frequently than policy updates.
2. Deleted codes and codes which are not effective at the time the service is rendered may
not be eligible for reimbursement.
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
CPT
®
*
Codes
Description
19316
Mastopexy
19318
Breast reduction
Considered integral to and not separately reimbursed when performed with a Medically
Necessary breast reduction:
CPT
®
*
Codes
Description
15877
Suction assisted lipectomy; trunk
19350
Nipple/areola reconstruction
Considered Cosmetic/Not Medically Necessary:
CPT
®
*
Codes
Description
19355
Correction of inverted nipples
Considered Unproven when performed as a sole method of treatment for symptomatic
macromastia:
CPT
®
*
Codes
Description
15877
Suction assisted lipectomy; trunk
*Current Procedural Terminology (CPT
®
) ©2023 American Medical Association: Chicago,
IL.

Page 9 of 13
Medical Coverage Policy: 0152
References
1. Amaral MH, Dao H, Shin JH. Racial and socioeconomic disparities in reduction
mammoplasty: an analysis of nationwide inpatient sample database. Ann Plast Surg. 2011
May;66(5):476-8. doi: 10.1097/SAP.0b013e3182185efa. PMID: 21451367.
2. American College of Obstetricians and Gynecologists (ACOG). Committee Opinion No. 686:
Breast and Labial Surgery in Adolescents. Obstet Gynecol. 2017 Jan;129(1):e17-e19. doi:
10.1097/AOG.0000000000001862. PMID: 28002312.
3. American Society of Plastic Surgeons (ASPS). Reduction Mammaplasty Recommended
Insurance Coverage for Third-Party Payer Coverage. May 2011. Updated Reaffirmed: Mar
2021. Accessed Jul 9, 2024. Available at URL address: https://www.plasticsurgery.org/for-
medical-professionals/health-policy/recommended-insurance-coverage-criteria
4. American Society of Plastic Surgeons. Reconstructive Procedures: Breast Reduction,
Reduction Mammaplasty. 2023. Accessed Jun 27, 2023. Available at URL address:
https://www.plasticsurgery.org/reconstructive-procedures/breast-reduction
5. Ayhan S, Basterzi Y, Yavuzer R, Latifoglu O, Cenetoglu S, Atabay K, Celebi MC. Histologic
profiles of breast reduction specimens. Anesthetic Plast Surg. 2002 May;26(3):203-5.
6. Banikarim C, DeSilva N. Breast disorders in children and adolescents. In: UpToDate, Drutz
JE and Middleman AB (Eds.). Feb 10, 2022. UpToDate, Waltham, MA. Accessed Jun 27,
2023.
7. Bellini E, Grieco MP, Raposio E. A journey through liposuction and liposculture: Review. Ann
Med Surg (Lond). 2017 Nov 6;24:53-60.
8. Blomqvist L, Brandberg Y. Three-year follow-up on clinical symptoms and health-related
quality of life after reduction mammaplasty Plast Reconstr Surg. 2004 Jul;114(1):49-54.
9. Bruhlmann Y, Tschopp H. Breast reduction improves symptoms of macromastia and has a
long-lasting effect. Ann Plast Surg. 1998 Sep;41(3):240-5.
10. Centers for Medicare and Medicaid Services (CMS). Local Coverage Determinations (LCDs)
alphabetical index. Accessed Jun 27, 2023. Available at URL address:
https://www.cms.gov/medicare-coverage-database/reports/local-coverage-final-lcds-
alphabetical-report.aspx?lcdStatus=all
11. Centers for Medicare and Medicaid Services (CMS). National Coverage Determinations
(NCDs) alphabetical index. Accessed Jun 27, 2023. Available at URL address:
https://www.cms.gov/medicare-coverage-database/reports/national-coverage-ncd-
report.aspx?chapter=all&sortBy=title
12. Chadbourne EB, Zhang S, Gordon MJ, Ro EY, Ross SD, Schnur PL, Schneider-Redden PR.
Clinical outcomes in reduction mammoplasty: a systematic review and meta-analysis of
published studies. Mayo Clin Proc. 2001 May;76(5):503-10.
13. Chao JD, Memmel HC, Redding JF, Egan L, Odom LC, Casas LA. Reduction mammaplasty is
a functional operation, improving quality of life in symptomatic women: a prospective,
Page 10 of 13
Medical Coverage Policy: 0152
single-center breast reduction outcome study. Plast Reconstr Surg. 2002 Dec;110(7):1644-
52.
14. Cohen R. Mastopexy options and techniques. Nahabedian MY, editor. In: Plastic Surgery,
Volume 5: Breast, 4
th
ed. Philadelphia, PA: Elsevier; 2018. Ch 6, 87-107.e1
15. Collins ED, Kerrigan CL, Kim M. The effectiveness of surgical and nonsurgical interventions
in relieving the symptoms of macromastia. Plast Reconstr Surg. 2002 Jul;109:1556-66.
16. Conner LN, Merritt DF. Breast Concerns. In: Kliegman RM, Stanton BF, St Geme JW, Schor
NF, Behrman RE, editors. Kliegman: Nelson Textbook of Pediatrics. 21
th
ed. Philadelphia,
PA: Elsevier; 2020. Ch 556, Breast Concerns, 2853-57.
17. Cunningham BL, Gear AJ, Kerrigan CL, Collins ED. Analysis of breast reduction
complications derived from the BRAVO study. Plast Reconstr Surg. 2005 May;115(6):1597-
604.
18. DeSilva NK, Brandt ML. Disorders of the breast in children and adolescents, Part 1:
Disorders of growth and infections of the breast. J Pediatr Adolesc Gynecol. 2006
Oct;19(5):345-9.
19. Economides JM, Graziano F, Tousimis E, Willey S, Pittman TA. Expanded Algorithm and
Updated Experience with Breast Reconstruction Using a Staged Nipple-Sparing Mastectomy
following Mastopexy or Reduction Mammaplasty in the Large or Ptotic Breast. Plast
Reconstr Surg. 2019 Apr;143(4):688e-697e. doi: 10.1097/PRS.0000000000005425.
Erratum in: Plast Reconstr Surg. 2019 Jun;143(6):1810-1811. PMID: 30921113.
20. Gonzalez MA, Glickman LT, Aladegbami B, Simpson RL. Quality of life after breast reduction
surgery: a 10-year retrospective analysis using the Breast Q questionnaire: does breast
size matter? Ann Plast Surg. 2012 Oct;69(4):361-3.
21. Greydanus DE, Matytsina L, Gains M. Breast Disorders in Children and Adolescents. Prim
Care. 2006 Jun;33(2):455-502.
22. Gunnarsson GL, Bille C, Reitsma LC, Wamberg P, Thomsen JB. Prophylactic Nipple-Sparing
Mastectomy and Direct-to-Implant Reconstruction of the Large and Ptotic Breast: Is
Preshaping of the Challenging Breast a Key to Success? Plast Reconstr Surg. 2017
Sep;140(3):449-454. doi: 10.1097/PRS.0000000000003621. PMID: 28841601.
23. Hansen J, Chang S. Overview of breast reduction. In: UpToDate, Chagpar AB, Colwell AS
(Ed). Last updated Apr 19, 2023. UpToDate, Waltham, MA. Accessed Jul 9, 2024.
24. Haug V, Kadakia N, Wang AT, Dorante MI, Panayi AC, Kauke-Navarro M, Hundeshagen G,
Diehm YF, Fischer S, Hirche C, Kneser U, Pomahac B. Racial disparities in short-term
outcomes after breast reduction surgery-A National Surgical Quality Improvement Project
Analysis with 23,268 patients using Propensity Score Matching. J Plast Reconstr Aesthet
Surg. 2022 Jun;75(6):1849-1857. doi: 10.1016/j.bjps.2022.01.001. Epub 2022 Jan 16.
PMID: 35131191.
25. Jakubietz RG, Jakubietz DF, Gruenert JG, Schmidt K, Meffert RH, Jakubietz MG. Breast
reduction by liposuction in females. Aesthetic Plast Surg. 2011 Jun;35(3):402-7.
Page 11 of 13
Medical Coverage Policy: 0152
26. Kalliainen LK; ASPS Health Policy Committee. ASPS clinical practice guideline summary on
reduction mammaplasty. Plast Reconstr Surg. 2012 Oct;130(4):785-9.
27. Killelea B and Sowden M. Nipple inversion. In: UpToDate, Chen W, ed. Feb 7, 2024.
UpToDate, Walthem, MA. Accessed Jul 9, 2024.
28. Kim DK, Ascherman JA. Impact of Sociodemographic and Hospital Factors on Inpatient
Bilateral Reduction Mammaplasty: A National Inpatient Sample Analysis. Plast Reconstr
Surg Glob Open. 2024 Mar 22;12(3):e5682.
29. Kocak E, Carruthers KH, McMahan JD. A reliable method for the preoperative estimation of
tissue to be removed during reduction mammaplasty. Plast Reconstr Surg. 2011
Mar;127(3):1059-64.
30. Manahan MA, Buretta KJ, Chang D, Mithani SK, Mallalieu J, Shermak MA. An outcomes
analysis of 2142 breast reduction procedures. Ann Plast Surg. 2015 Mar;74(3):289-92.
31. McGrath MH, Pomerantz J. Plastic Surgery. Reduction Mammoplasty. In: Townsend CM,
Beuchamp RD, Evers BM, editors. Townsend: Sabiston Textbook of Surgery, 19
th
ed.
Philadelphia, PA: WB Saunders Company. 2012. pg 1932-33. Ch 69.
32. McGrath MH, Schooler WG. Elective plastic surgical procedures in adolescence. Adolesc Med
Clin. 2004 Oct;15(3):487-502.
33. Morris MP, Christopher AN, Patel V, Broach RB, Fischer JP, Butler PD. Assessing Disparities
in Reduction Mammaplasty: There Is Room for Improvement. Aesthet Surg J. 2021 Jun
14;41(7):NP796-NP803. doi: 10.1093/asj/sjab138. PMID: 33735387.
34. Moskovitz MJ, Baxt SA, Jain AK, Hausman RE. Liposuction breast reduction: a prospective
trial in African American women. Plast Reconstr Surg. 2007 Feb;119(2):718-26; discussion
727-8.
35. Nahai FR, Nahai F. MOC-PSSM CME article: Breast reduction. Plast Reconstr Surg. 2008
Jan;121(1 Suppl):1-13.
36. National Comprehensive Cancer Network
®
(NCCN). NCCN GUIDELINES™ Clinical Practice
Guidelines in Oncology
™
.
©
Breast Cancer Risk Reduction. Version 2.2024 Mar 11, 2024.
National Comprehensive Cancer Network, Inc. 2024, All Rights Reserved. Accessed Jul 9,
2024. Available at URL address:
https://www.nccn.org/professionals/physician_gls/pdf/breast_risk.pdf
37. National Comprehensive Cancer Network
®
(NCCN). NCCN GUIDELINES™ Clinical Practice
Guidelines in Oncology
™
. Genetic/Familial High-risk Assessment: Breast, Ovarian, and
Pancreatic. Version 3.2024 Feb 12, 2024. National Comprehensive Cancer Network, Inc.
2022, All Rights Reserved. Accessed Jul 9, 2024. Available at URL address:
https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf
38. Perdikis G, Dillingham C, Boukovalas S, Ogunleye AA, Casambre F, Dal Cin A, Davidson C,
Davies CC, Donnelly KC, Fischer JP, Johnson DJ, Labow BI, Maasarani S, Mullen K, Reiland
J, Rohde C, Slezak S, Taylor A, Visvabharathy V, Yoon-Schwartz D. American Society of
Plastic Surgeons Evidence-Based Clinical Practice Guideline Revision: Reduction
Mammaplasty. Plast Reconstr Surg. 2022 Mar 1;149(3):392e-409e. doi:
10.1097/PRS.0000000000008860. PMID: 35006204.
Page 12 of 13
Medical Coverage Policy: 0152
39. Pu LLQ. Breast Reduction—Medial Pedicle Technique. Pu LLQ and Jewell ML, eds. In: Atlas
of Contemporary Aesthetic Breast Surgery, Elsevier Inc. 2021. Ch 18, 249-258.
40. Redlarski G, Palkowski A, Krawczuk M. Body surface area formulae: an alarming ambiguity.
Sci Rep. 2016 Jun 21;6:27966. doi: 10.1038/srep27966. PMID: 27323883; PMCID:
PMC4914842.
41. Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976 Apr;3(2):193-
203. PMID: 1261176.
42. Sadove R. New observations in liposuction-only breast reduction. Aesthetic Plast Surg.
2005 Jan-Feb;29(1):28-31.
43. Salibian AA, Frey JD, Karp NS, Choi M. Does Staged Breast Reduction before Nipple-
Sparing Mastectomy Decrease Complications? A Matched Cohort Study between Staged
and Nonstaged Techniques. Plast Reconstr Surg. 2019 Nov;144(5):1023-1032. doi:
10.1097/PRS.0000000000006121. PMID: 31373992.
44. Schnur PL, Hoehn JG, Ilstrup DM, Cahoy MJ, Chu CP. Reduction mammaplasty: cosmetic or
reconstructive procedure? Ann Plast Surg. 1991 Sep;27(3):232-7.
45. Schnur PL, Schnur DP, Petty PM, Hanson TJ, Weaver Al. Reduction mammoplasty: an
outcome study. Plast Reconstr Surg. 1997 Sep;100(4):875-83.
46. Singh KA, Losken A. Additional benefits of reduction mammaplasty: a systematic review of
the literature. Plast Reconstr Surg. 2012 Mar;129(3):562-70.
47. Souto GC, Giugliani ER, Giugliani C, Schneider MA. The impact of breast reduction surgery
on breastfeeding performance. J Hum Lact. 2003 Feb;19(1):43-9;quiz 66-9, 120.
48. Spear SL, Rottman SJ, Seiboth LA, Hannan CM. Breast reconstruction using a staged
nipple-sparing mastectomy following mastopexy or reduction. Plast Reconstr Surg. 2012
Mar;129(3):572-581. doi: 10.1097/PRS.0b013e318241285c. PMID: 22373964.
49. Tondu T, Thiessen F, Hubens G, Tjalma W, Blondeel P, Verhoeven V. Delayed two-stage
nipple sparing mastectomy and simultaneous expander-to-implant reconstruction of the
large and ptotic breast. Gland Surg. 2022 Mar;11(3):524-534. doi: 10.21037/gs-21-734.
PMID: 35402205; PMCID: PMC8984988.
50. Zhang MX, Chen CY, Fang QQ, Xu JH, Wang XF, Shi BH, Wu LH, Tan WQ. Risk Factors for
Complications after Reduction Mammoplasty: A Meta-Analysis. PLoS One. 2016 Dec
9;11(12):e0167746.
Revision Details
Type of Revision
Summary of Changes
Date
Annual review
• No clinical policy statement changes
8/15/2024

Page 13 of 13
Medical Coverage Policy: 0152
“Cigna Companies” refers to operating subsidiaries of The Cigna Group. All products and services
are provided exclusively by or through such operating subsidiaries, including Cigna Health and Life
Insurance Company, Connecticut General Life Insurance Company, Evernorth Behavioral Health,
Inc., Cigna Health Management, Inc., and HMO or service company subsidiaries of The Cigna
Group. © 2024 The Cigna Group.
